
How to Cure Irritable Bowel Syndrome Naturally with Functional Medicine?
June 10, 2025Your digestive system is often called the “second brain” — and for good reason. It handles breaking down everything you eat, extracting vital nutrients, managing trillions of microbes (your gut microbiome), and sending signals that affect your immune system, hormones, and even your mood.
When your gut is unhealthy, you might notice symptoms like bloating, stomach pain, fatigue, or even brain fog and skin problems. These are not isolated issues but clues your body gives when the digestive system is out of balance.
Most conventional medicine focuses on treating symptoms — like popping antacids for heartburn or anti-diarrheal pills for upset stomach — but functional medicine takes a different path. It seeks to understand the root cause of the digestive issues and restore true health by optimizing digestion and healing the gut naturally.
Dr. Monica Bhardwaj, a renowned functional medicine practitioner, uses this approach to help patients regain their health holistically, by combining modern science with personalized, natural therapies.
Meet Dr. Monica Bhardwaj: The Functional Medicine Pioneer in Digestive Health
Dr. Monica Bhardwaj is a pioneer in the functional medicine space, focusing on digestive wellness as the foundation for overall health. Her approach is different because she looks beyond just symptoms and routine tests. Instead, she:
- Uses advanced diagnostic tools like stool analysis, breath tests, and food sensitivity panels that reveal hidden imbalances.
- Creates a personalized treatment plan based on your unique biology, environment, and lifestyle.
- Prescribes natural interventions such as herbal supplements, nutritional therapies, and gut-healing nutrients.
- Recognizes the importance of mental health and stress, incorporating mind-body therapies to restore the gut-brain connection.
- Educates and empowers her patients to understand their bodies and take an active role in their healing journey.
By addressing all aspects of health, Dr. Monica’s functional medicine approach offers long-lasting solutions instead of quick fixes.
The Top 5 Digestive Health Issues You Must Know About
1. Irritable Bowel Syndrome (IBS)

What is IBS?
IBS is a common digestive disorder characterized by a cluster of symptoms including abdominal cramping, bloating, and irregular bowel habits such as diarrhea, constipation, or both. It can significantly affect quality of life and is often misunderstood.
Why does IBS occur?
IBS is caused by multiple interlinked factors:
- Microbial imbalance: Your gut houses both helpful and harmful bacteria. In IBS, harmful bacteria or yeast may overgrow, upsetting digestion and causing gas and bloating.
- Food sensitivities: Many IBS sufferers react to specific fermentable carbs called FODMAPs (found in garlic, onions, wheat, apples), gluten, or dairy, leading to digestive upset.
- Gut-brain axis disruption: Stress and anxiety can worsen symptoms by altering gut motility and increasing pain perception.
- Low-grade inflammation: Inflammation in the gut lining may make the intestines hypersensitive.
How Dr. Monica Bhardwaj Tackles IBS:
- Comprehensive Testing: She uses stool and breath tests to pinpoint microbial imbalances, yeast overgrowth, or hidden infections causing IBS symptoms.
- Personalized Elimination Diets: She guides you to identify and remove foods that trigger symptoms, often starting with a low-FODMAP or gluten-free diet tailored to your body.
- Rebalancing the Microbiome: With targeted probiotics and prebiotics, she helps repopulate good bacteria and restore balance.
- Calming the Nervous System: Mind-body practices such as guided meditation, breathing exercises, and yoga are integrated to reduce stress and normalize gut-brain communication.
- Reducing Inflammation: Natural anti-inflammatory supplements like turmeric, ginger, and omega-3 fatty acids are recommended to soothe the gut lining.
Extra Practical Tips:
- Keep a detailed food and symptom diary to spot patterns and avoid triggers.
- Engage in gentle daily exercise like walking, which helps regulate bowel movements.
- Avoid caffeine, alcohol, and carbonated drinks to reduce gut irritation.
2. Gastroesophageal Reflux Disease (GERD)

What is GERD?
GERD is the condition where stomach acid flows back into the esophagus, causing symptoms like:
- Heartburn (a burning sensation behind the breastbone)
- Regurgitation of acid or food
- Hoarseness, chronic cough, or a sour taste in the mouth
- Difficulty swallowing or chest discomfort
Why does GERD happen?
The main cause is a weakened or dysfunctional lower esophageal sphincter (LES) — the muscle that acts as a valve between the stomach and esophagus. Factors contributing include:
- Poor LES function allows acid reflux.
- Delayed stomach emptying increases pressure, forcing acid upward.
- Lifestyle factors: obesity, smoking, overeating, or lying down right after meals can worsen reflux.
- Interestingly, many people with GERD have low stomach acid, which causes incomplete digestion and leads to reflux symptoms.
Dr. Monica’s Functional Medicine Approach to GERD:
- Assessing Stomach Acid Levels: Through specialized tests, she determines if you have low stomach acid, a key but often overlooked cause of reflux.
- Supporting Digestion: Using natural bitters, digestive enzymes, and apple cider vinegar to improve stomach acid production and digestion.
- Gut Lining Repair: Supplements like L-glutamine, zinc carnosine, and slippery elm soothe and protect the esophageal lining from acid damage.
- Lifestyle Coaching: Guidance on eating smaller meals, avoiding trigger foods (spicy, fatty, chocolate, caffeine), and sleeping with the head elevated to reduce reflux episodes.
- Stress Management: Incorporating relaxation techniques, as stress increases acid secretion and muscle tension.
Extra Practical Tips:
- Avoid eating at least 3 hours before bedtime to reduce reflux risk.
- Maintain a healthy weight to lower abdominal pressure on the stomach.
- Quit smoking and limit alcohol to protect your LES function.
3. Small Intestinal Bacterial Overgrowth (SIBO)
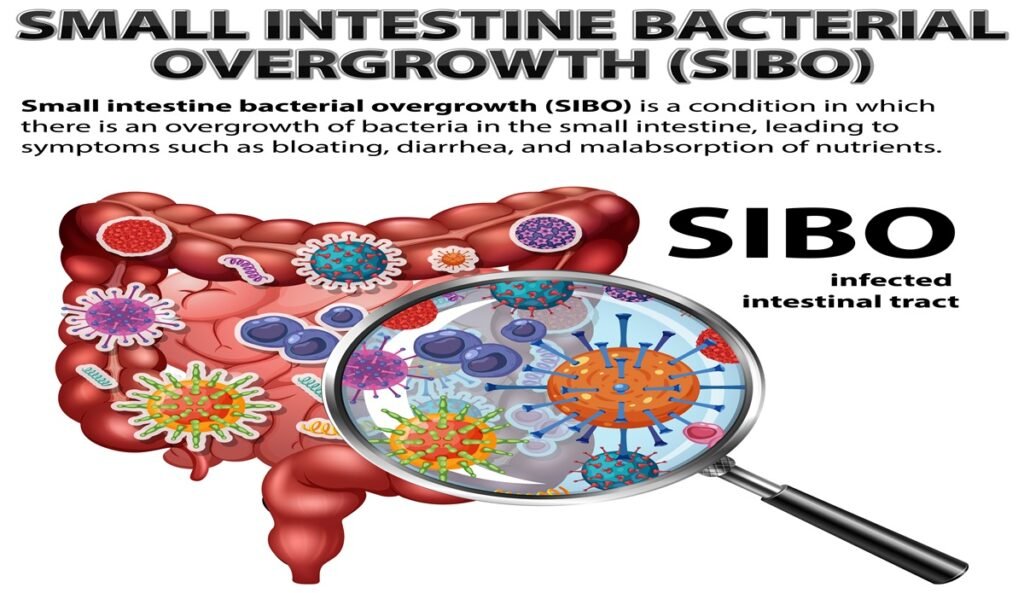
What is SIBO?
SIBO occurs when bacteria from the large intestine overgrow in the small intestine, where they are normally sparse. This causes:
- Excessive gas and bloating
- Abdominal discomfort
- Diarrhea, constipation, or alternating patterns
- Malabsorption of nutrients, leading to deficiencies and fatigue
Why does SIBO develop?
Several factors impair the small intestine’s natural defense:
- Low stomach acid: Allows bacteria to survive and multiply.
- Impaired gut motility: Slow movement means bacteria linger longer.
- Structural abnormalities: Surgeries, diverticula, or strictures can trap bacteria.
- Medication use: Proton pump inhibitors and antibiotics disturb the gut environment.
Dr. Monica’s Approach to SIBO:
- Diagnostic Breath Tests: Identifying whether hydrogen or methane-producing bacteria predominate helps tailor treatment.
- Herbal Antimicrobials: Natural agents like oregano oil, berberine, neem, and garlic selectively eliminate harmful bacteria while preserving beneficial ones.
- Improving Gut Motility: Using natural prokinetics like ginger, Iberogast, and magnesium to enhance intestinal clearing.
- Targeted Diets: Low-FODMAP or elemental diets reduce fermentable substrates feeding bacteria.
- Gut Healing: Post-treatment support with glutamine and probiotics to restore the gut lining and microbiome balance.
Extra Practical Tips:
- Avoid unnecessary antibiotics that can worsen dysbiosis.
- Gentle movement after meals promotes digestion and motility.
- Regular hydration keeps intestinal transit smooth.
4. Inflammatory Bowel Disease (IBD)
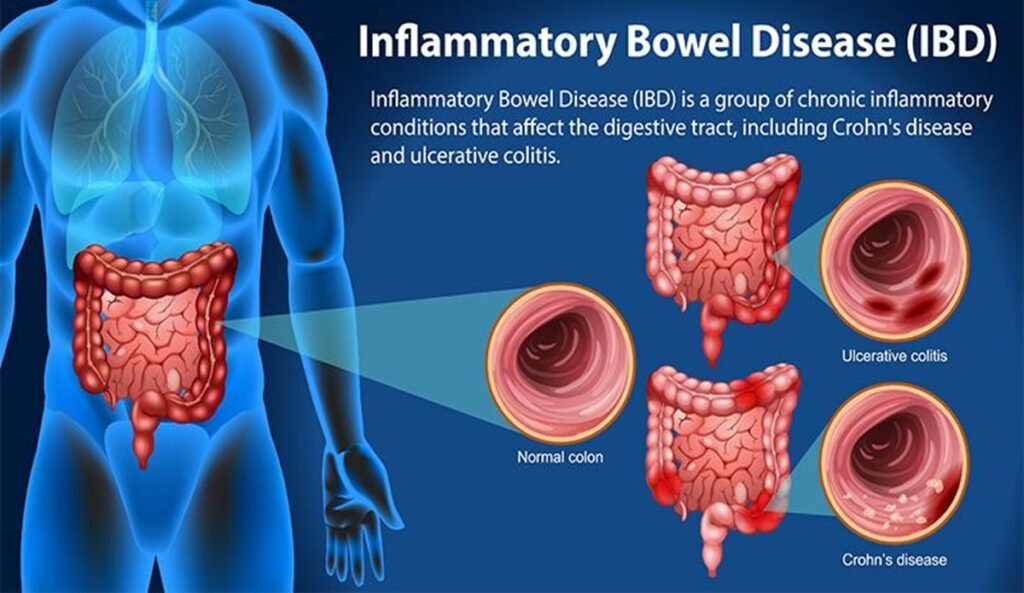
Source: Kottakkal Ayurveda
What is IBD?
IBD refers mainly to Crohn’s disease and ulcerative colitis, chronic conditions where the immune system attacks parts of the digestive tract, causing:
- Severe abdominal pain
- Persistent diarrhea, often bloody
- Weight loss and malnutrition
- Fatigue and anemia
- Risk of complications like strictures, abscesses, or colon cancer
Why does IBD develop?
IBD is complex and involves:
- Genetic susceptibility
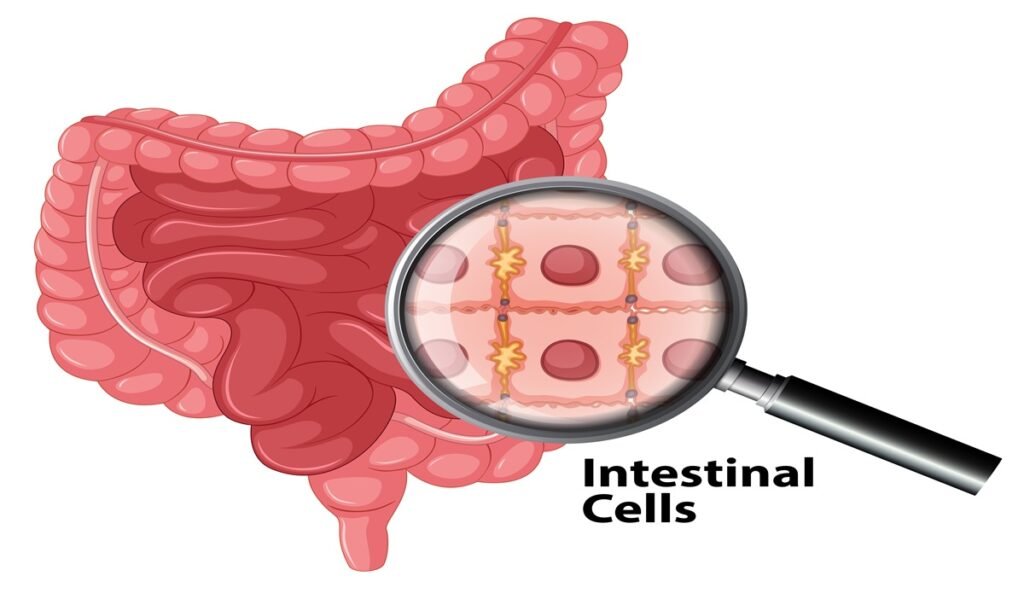
- Immune system dysfunction, with chronic inflammation damaging the gut lining
- Microbiome imbalances exacerbating inflammation
- Environmental triggers such as smoking, stress, and diet
Dr. Monica’s Functional Medicine Strategy for IBD:
- Anti-inflammatory Nutrition: Diets rich in omega-3 fatty acids (fish, flaxseeds), antioxidant-packed fruits and vegetables, and avoidance of processed foods help modulate immune responses.
- Targeted Supplements: Curcumin, vitamin D, and probiotics to reduce inflammation and support gut flora.
- Gut Barrier Repair: Nutrients like collagen peptides, bone broth, zinc, and L-glutamine help rebuild the intestinal lining to reduce “leaky gut” and immune activation.
- Stress Reduction: Mindfulness, meditation, and other mind-body therapies lower flare-up risk by calming immune overactivity.
- Integrated Care: Working alongside specialists, Dr. Monica ensures your treatment plan is comprehensive and personalized.
Extra Practical Tips:
- Avoid sugar, processed foods, and artificial additives that trigger inflammation.
- Engage in moderate physical activity regularly to balance immune function.
- Prioritize good sleep for immune regulation.
5. Intestinal Infections
What are intestinal infections?
These are caused by harmful bacteria, viruses, or parasites invading your gut, resulting in symptoms like:
- Sudden diarrhea
- Abdominal cramps
- Nausea and vomiting
- Fever and dehydration
Why do intestinal infections happen?
Common causes include:
- Contaminated food or water
- Poor hygiene or travel to high-risk areas
- Weakened immune defenses
Dr. Monica’s Functional Medicine Approach:
- Natural Antimicrobials: Herbal remedies such as garlic, neem, oregano oil, and goldenseal target pathogens effectively without wiping out healthy bacteria.
- Hydration Support: Using electrolyte-rich fluids to prevent dehydration during illness.
- Microbiome Restoration: Probiotic supplementation and prebiotic foods help re-establish beneficial gut flora after infection.
- Gut Lining Healing: Nutrients like zinc and L-glutamine repair damage to the intestinal walls and reduce permeability.
- Immune Support: Nutritional guidance to strengthen immunity and speed recovery.
Extra Practical Tips:
- Always wash hands thoroughly and avoid risky foods when traveling.
- Rest sufficiently to help your immune system fight off infection.
- Practice safe food handling at home.
How Functional Medicine Works: The Dr. Monica Bhardwaj Difference
Functional medicine is not just about symptom suppression; it’s about healing your body at the root level. Here’s what sets Dr. Monica’s approach apart:
- Detailed Diagnostic Testing: Routine tests often miss subtle imbalances. Dr. Monica uses advanced stool, breath, and blood tests to uncover hidden infections, food sensitivities, and nutrient gaps.
- Personalized Care: No two guts are alike. Treatment plans are tailored precisely to your biology, preferences, and lifestyle.
- Natural Healing Focus: Herbs, supplements, and nutrition support your body’s innate ability to repair itself without harsh drugs or side effects.
- Holistic Support: Mental and emotional health are recognized as key factors in digestive wellness. Stress reduction and mind-body therapies are integral.
- Ongoing Guidance: Healing takes time. Dr. Monica provides continuous monitoring and adjustments to ensure lasting results.
Quick Interactive Self-Check: How Healthy Is Your Gut?
Ask yourself:
- Do you often experience bloating or gas after meals?
- Are your bowel movements irregular or painful?
- Do you feel fatigued or have difficulty concentrating?
- Do certain foods consistently upset your stomach?
- Do you suffer from frequent heartburn or acid reflux?
If you answered yes to any, it may be time to explore a functional medicine approach for healing.
Dr. Monica’s 7 Easy Tips to Nurture Your Digestive Health Every Day
- Choose Whole, Unprocessed Foods: Focus on fiber-rich fruits, vegetables, nuts, and seeds that feed your good gut bacteria and keep digestion smooth.
- Stay Hydrated: Water helps flush toxins and keeps your digestive tract functioning optimally.
- Chew Your Food Thoroughly: Proper chewing initiates digestion and reduces the burden on your stomach and intestines.
- Manage Stress: Practices like deep breathing, meditation, and yoga calm your nervous system and improve gut-brain communication.
- Avoid Unnecessary Medications: Antibiotics and NSAIDs can harm your gut flora and lining; use them only when essential.
- Eat Fermented Foods Regularly: Yogurt, kimchi, sauerkraut, and kefir introduce beneficial bacteria to your gut ecosystem.
- Prioritize Quality Sleep: Sleep allows your gut to repair and regenerate; aim for 7–9 hours nightly.
Final Thoughts: Your Gut Is the Gateway to True Wellness
Digestive health is foundational to feeling your best. Chronic digestive issues don’t have to control your life. Dr. Monica Bhardwaj’s functional medicine approach offers a personalized, natural roadmap to heal your gut, reduce symptoms, and improve your overall vitality.
Take the first step toward a healthier, happier gut — and life. Your body will thank you.
Explore how Dr. Monica’s expert care can help you unlock true digestive wellness today.
Further Reading & Trusted Sources
- University of Chicago Medicine – Common Digestive Conditions
- Gastro London – Natural Remedies for IBS
- Pace Hospital – Home Remedies for Intestinal Infection
- [Cleveland Clinic – Gastrointestinal Diseases](https://my.clevelandclinic.org/health/diseases/4237-inflammatory-bowel-disease-ibd)


